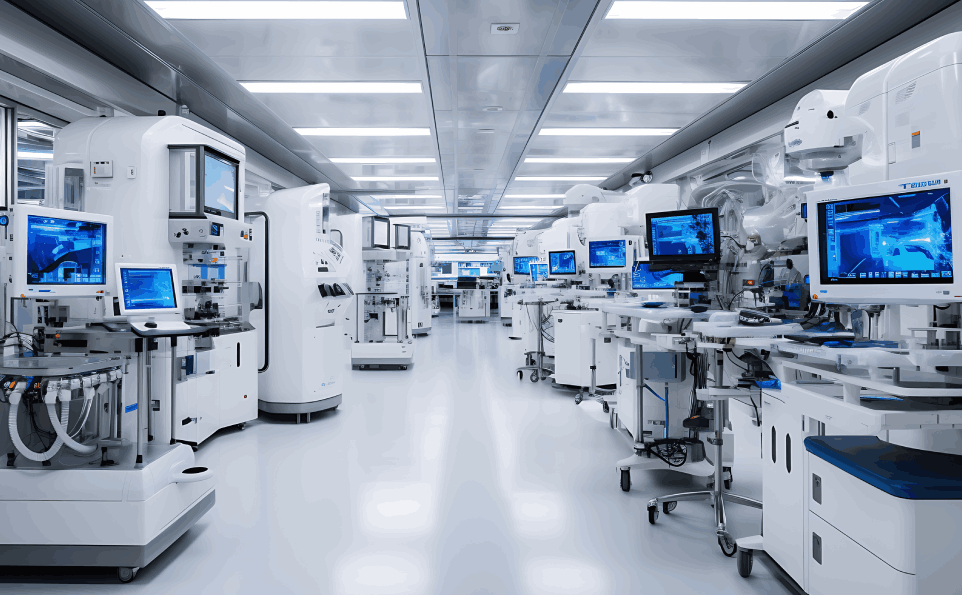
Medical devices play a crucial role in modern healthcare, significantly enhancing the ability to diagnose, treat, and manage various health conditions. From simple instruments like thermometers to complex machinery such as MRI scanners, medical devices are indispensable in ensuring effective patient care. However, with their widespread use comes the critical responsibility of ensuring their safety and efficacy. This is where regulatory compliance becomes essential, serving as a safeguard for patient safety and a benchmark for quality assurance in the medical device industry.
Regulatory compliance involves adhering to the rules, guidelines, and standards set by regulatory bodies to ensure that medical devices are safe for use and perform as intended. Compliance is not merely a legal requirement but a commitment to upholding the highest standards of patient care. It encompasses various aspects, including device classification, clinical trial requirements, and quality management systems (QMS). Navigating this complex regulatory landscape is a significant challenge for manufacturers, necessitating a strategic approach to ensure both compliance and market success.
The Complex Regulatory Landscape
A. Global Market, Varied Regulations
The medical device industry operates on a global scale, with products being distributed and used in diverse markets. Each market has its own regulatory framework, creating a multifaceted and challenging landscape for manufacturers. Key regulatory bodies include the U.S. Food and Drug Administration (FDA), which oversees the approval and monitoring of medical devices in the United States; the European Union’s CE marking system, which signifies compliance with EU safety, health, and environmental requirements; and the China Food and Drug Administration (CFDA), responsible for regulating medical devices in China.
Complying with these varied regulations is a formidable task. Each regulatory body has its own set of standards, documentation requirements, and approval processes. For instance, a device approved by the FDA might still require substantial additional work to meet the standards set by the CE marking system. This necessitates a comprehensive understanding of the regulatory requirements in each target market and often requires localized strategies to address specific regulatory demands.
B. Ever-Evolving Standards
The regulatory landscape for medical devices is dynamic, with standards and requirements continually evolving. Advances in technology, new scientific discoveries, and emerging health threats necessitate regular updates to regulatory guidelines. For manufacturers, this means that compliance is not a one-time effort but an ongoing process that requires vigilance and adaptability.
Staying informed about changes in regulations and standards is crucial. Manufacturers must be proactive in updating their procedures, documentation, and training programs to reflect the latest requirements. This ongoing adaptation is essential not only for maintaining compliance but also for leveraging new opportunities in the market and ensuring that their devices continue to meet the highest safety and performance standards.
Key Regulatory Hurdles
A. Classification of Medical Devices
Medical devices are classified into different categories based on their risk profile and intended use. These classifications determine the regulatory pathways and requirements for each device. For instance, in the United States, the FDA classifies devices into three classes:
Class I: Low-risk devices such as bandages and handheld surgical instruments. These devices typically require general controls and are subject to the least regulatory oversight.
Class II: Moderate-risk devices such as infusion pumps and diagnostic ultrasound machines. These devices require general controls and special controls, which may include performance standards, postmarket surveillance, and specific labeling requirements.
Class III: High-risk devices such as pacemakers and heart valves. These devices require the most stringent regulatory controls, including premarket approval (PMA) and extensive clinical testing to ensure their safety and effectiveness.
The classification process considers various factors, including the device’s intended use, the duration of contact with the body, and the potential risks associated with its use. Understanding these classifications and their implications is critical for manufacturers, as it influences the regulatory strategy, the type and extent of clinical evidence required, and the overall timeline for bringing a device to market.
B. Clinical Trial Requirements
Clinical trials are a fundamental component of the regulatory approval process for many medical devices, particularly those classified as high-risk. Well-designed and conducted clinical trials provide the evidence needed to demonstrate the safety and efficacy of a device. These trials must adhere to rigorous ethical standards and prioritize patient safety.
The design of clinical trials should be robust, incorporating appropriate controls, adequate sample sizes, and relevant endpoints. Ethical considerations are paramount, including informed consent, protection of patient privacy, and the minimization of risks to participants. Regulatory bodies such as the FDA and the European Medicines Agency (EMA) have specific guidelines for conducting clinical trials, and compliance with these guidelines is essential for obtaining regulatory approval.
C. Quality Management Systems (QMS)
A robust Quality Management System (QMS) is crucial for the design, development, and manufacturing of medical devices. A QMS ensures that products consistently meet regulatory requirements and quality standards. Key elements of a QMS include:
Risk Management: Identifying, assessing, and mitigating risks associated with the device throughout its lifecycle. This includes conducting risk analyses, implementing control measures, and continuously monitoring and reviewing risks.
Documentation Control: Maintaining comprehensive and accurate documentation for all processes, procedures, and activities. This includes design history files, technical files, and quality records, which are essential for regulatory audits and inspections.
Design and Development Controls: Implementing systematic procedures for design and development activities to ensure that devices meet user needs and regulatory requirements. This includes design planning, design verification and validation, and design reviews.
Implementing and maintaining an effective QMS is a cornerstone of regulatory compliance, facilitating the consistent production of safe and effective medical devices.
Strategies for Successful Navigation
A. Building a Compliance Culture
Creating a culture of compliance within an organization is fundamental to navigating the regulatory landscape successfully. This involves fostering a company-wide commitment to regulatory adherence and quality assurance. Key strategies include:
Ongoing Training and Education: Regularly training all personnel involved in the design, development, manufacturing, and marketing of medical devices. This ensures that employees are aware of the latest regulatory requirements and understand their roles in maintaining compliance.
Leadership Commitment: Demonstrating top management’s commitment to regulatory compliance by allocating necessary resources, establishing clear policies, and leading by example. Leadership plays a crucial role in setting the tone for a compliance-oriented culture.
B. Partnering with Regulatory Experts
Collaborating with regulatory experts can significantly enhance a company’s ability to navigate complex approval processes. Regulatory consultants and advisors bring specialized knowledge and experience, providing valuable insights into regulatory requirements and strategies for compliance.
Guidance and Support: Regulatory experts can assist in developing regulatory strategies, preparing submission documents, and addressing regulatory queries. Their expertise helps in avoiding common pitfalls and expediting the approval process.
Staying Informed: Regulatory consultants are often well-versed in the latest developments in the regulatory landscape, helping manufacturers stay informed about changes and updates that may impact their products.
C. Proactive Risk Management
Effective risk management is essential for demonstrating the safety and efficacy of medical devices to regulatory bodies. Proactive risk management involves identifying and mitigating potential risks associated with the device throughout its lifecycle.
Risk Management Plans: Developing comprehensive risk management plans that outline strategies for identifying, assessing, and controlling risks. These plans should be integrated into the QMS and regularly reviewed and updated.
Continuous Monitoring: Implementing systems for ongoing monitoring and evaluation of risks, including postmarket surveillance and feedback mechanisms. This helps in promptly identifying and addressing any emerging safety concerns.
Conclusion
Navigating regulatory compliance in the medical device industry is a complex and ongoing challenge. Understanding the varied regulatory requirements across global markets, staying informed about evolving standards, and addressing key regulatory hurdles such as device classification, clinical trial requirements, and quality management systems are essential for successful compliance.
Building a compliance culture within the organization, partnering with regulatory experts, and adopting proactive risk management strategies are critical for navigating this complex landscape. Successful regulatory compliance not only ensures patient safety and device efficacy but also enhances market access, fosters patient trust, and ultimately contributes to the long-term success of medical device manufacturers.
By prioritizing regulatory compliance and adopting a strategic approach, manufacturers can effectively navigate the intricate regulatory environment, bringing safe and innovative medical devices to market and improving healthcare outcomes worldwide.
FAQs: Navigating Regulatory Compliance in the Medical Device Industry
Q1: What is regulatory compliance in the medical device industry?
A1: Regulatory compliance involves adhering to the rules, guidelines, and standards set by regulatory bodies to ensure medical devices are safe and effective. It includes meeting requirements for device classification, clinical trials, quality management systems, and ongoing monitoring.
Q2: Why is regulatory compliance important for medical devices?
A2: Regulatory compliance is crucial for ensuring patient safety, maintaining product efficacy, and meeting legal requirements. It helps in gaining market access, building patient trust, and avoiding legal and financial penalties.
Q3: What are the key regulatory bodies in the medical device industry?
A3: Key regulatory bodies include the U.S. Food and Drug Administration (FDA), the European Union’s CE marking system, and the China Food and Drug Administration (CFDA). Each has its own set of standards and requirements.
Q4: How are medical devices classified?
A4: Medical devices are classified based on their risk profile and intended use. In the U.S., the FDA classifies devices into Class I (low risk), Class II (moderate risk), and Class III (high risk). The classification determines the regulatory pathway and requirements for each device.
Q5: What are the clinical trial requirements for medical devices?
A5: Clinical trials are required to provide evidence of a device’s safety and efficacy. They must be well-designed, ethically conducted, and comply with guidelines set by regulatory bodies. This includes obtaining informed consent and ensuring patient safety.
Q6: What is a Quality Management System (QMS) and why is it important?
A6: A QMS is a set of policies and procedures for ensuring the quality and safety of medical devices throughout their lifecycle. Key elements include risk management, documentation control, and design and development controls. A robust QMS is essential for regulatory compliance and consistent product quality.
Q7: How can companies stay informed about evolving regulatory standards?
A7: Companies can stay informed by subscribing to updates from regulatory bodies, attending industry conferences, participating in professional organizations, and collaborating with regulatory consultants. Regular training and internal audits also help in keeping up with changes.
Q8: What are the benefits of partnering with regulatory experts?
A8: Partnering with regulatory experts provides specialized knowledge and experience, helping companies navigate complex regulatory processes, prepare submission documents, and address regulatory queries. Experts also help stay updated with regulatory changes and avoid common pitfalls.
Q9: What is proactive risk management in the context of medical devices?
A9: Proactive risk management involves identifying, assessing, and mitigating potential risks associated with a medical device throughout its lifecycle. This includes developing risk management plans, implementing control measures, and continuously monitoring for new risks.
Q10: How can a company build a compliance culture?
A10: Building a compliance culture involves fostering a company-wide commitment to regulatory adherence and quality assurance. This includes regular training and education, leadership commitment, and integrating compliance into all aspects of the organization’s operations.
 Hospital Furniture
Hospital Furniture Medical Devices
Medical Devices MSR Products
MSR Products Office Furniture
Office Furniture